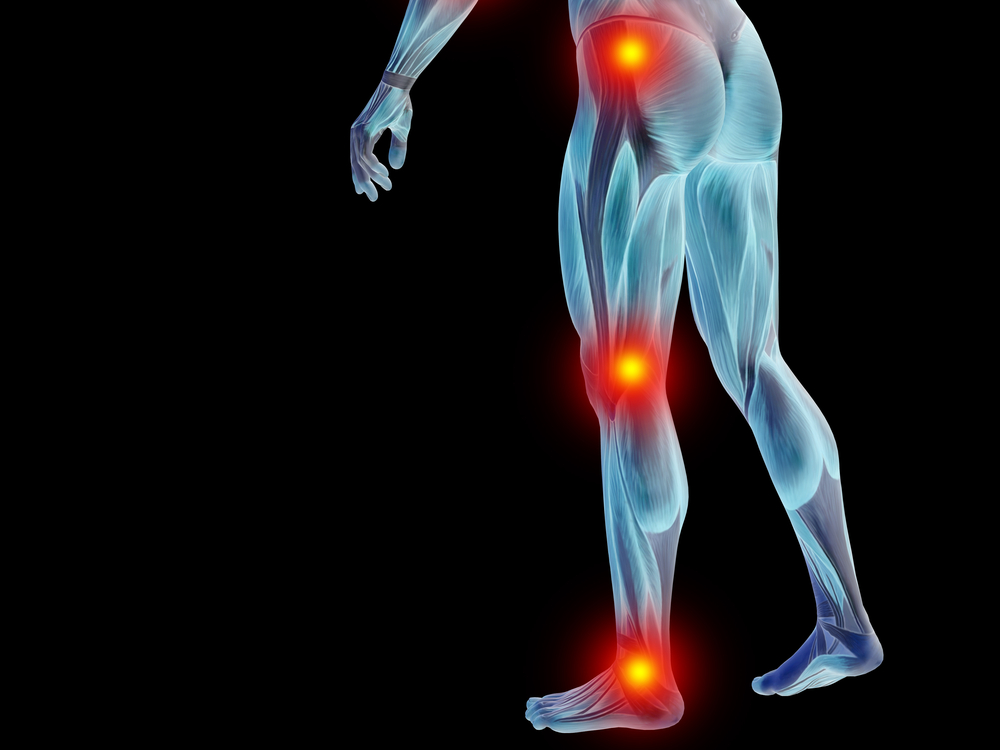
Spinal related leg pain refers to discomfort, aching, tingling, or numbness that radiates from the lumbar spine down the sciatic nerve into the legs. It is often caused by pressure on or damage to the nerve roots exiting the spinal cord.
Understanding what causes this pain and the anatomy involved provides insight into possible treatments. Getting an accurate diagnosis is also key to finding relief.
An Overview of Spinal Anatomy
The spine forms the main support structure of the body, protecting the spinal cord while allowing flexibility for movement. It consists of 33 vertebrae, including:
- 7 cervical vertebrae in the neck
- 12 thoracic vertebrae in the upper and mid back
- 5 lumbar vertebrae in the lower back
- 5 fused vertebrae forming the sacrum
- 4 fused vertebrae forming the tailbone
Between each vertebra are discs that act as cushions or shock absorbers. Facet joints link the vertebral bodies together, while tendons and muscles enable range of motion.
Spinal nerves exit between the vertebrae, branching out into the body to relay signals to and from the brain.
What Causes Spinal Related Leg Pain?
There are several potential causes of spinal related leg pain:
Nerve Compression
When spinal structures shift or press on nerves, it can interfere with proper signaling, causing pain, numbness, and weakness. Common culprits include:
Herniated Discs
- The jelly-like discs between vertebrae can bulge or rupture, pushing into the spinal canal. This compresses nerve roots, most often occurring in the lumbar spine.
Bone Spurs
- Extra bone growths called osteophytes can form around joints as cartilage breaks down. These spurs may narrow the spinal canal, putting pressure on nerves.
Spinal Tumors
- Noncancerous (benign) or cancerous (malignant) growths along the spine can similarly impinge nerves.
Structural Changes
Degenerative issues and misalignments also contribute to radiating discomfort:
Spinal Stenosis
- Wear-and-tear causes the open spaces in the spine to narrow. This puts pressure on the spinal cord and nerves, especially evident during activity.
Spondylolisthesis
- When a vertebra slips out of alignment, it can pinch nearby nerves. This often occurs in the lumbar region.
Sciatica
- Inflammation of the sciatic nerve, which runs from the lower back through the hips and butt, provokes shooting leg pains.
Inflammation
- Swelling and irritation around spinal joints and tissues can lead to nerve impingement:
Arthritis
- Joint inflammation from osteoarthritis and autoimmune types like rheumatoid arthritis causes bone spurs and swollen tissues pressing into nerves.
Infections
- Bacterial or fungal spinal infections prompt inflammation, abscesses, and pus formation, which can damage nerve roots.
Injuries
- Trauma to the spine also sets the stage for lasting nerve aggravation:
Accidents
- Car crashes, falls, sports impacts, and other injuries can fracture vertebrae or rupture discs, scarring nerve tissues.
What are the Symptoms?
Leg pain related to spinal nerve impingement produces several characteristic symptoms:
Sensory Symptoms
Compression prevents proper nerve signaling, causing uncomfortable sensations including:
Numbness
- Nerves fail to transmit typical sensations from the legs and feet. It may feel like limbs are “asleep.”
Tingling
- Pins and needles feelings result from impeded nerve communication.
Burning Pain
- Nerve inflammation produces a severe, hot discomfort that travels down the legs.
Motor Symptoms
Weakened nerve signaling interferes with muscle control:
Leg Weakness
- Signals don’t correctly relay to leg and foot muscles, causing difficulty moving normally.
Impaired Walking
- Foot drop or dragging can occur, along with imbalance and increased risk of falls.
Cramping
- Overactive signals produce painful involuntary muscle spasms.
How is Spinal Related Leg Pain Diagnosed?
To pinpoint the cause of radiating leg discomfort, doctors utilize:
Medical History
- Discussing symptoms, onset, relieving/worsening factors, family history, medications, other medical issues, etc. provides clues.
Physical Exam
- Checking reflexes, sensation, muscle strength and tone helps locate affected nerves.
Imaging Tests
- Seeing spinal structures helps identify sources of nerve compression like disc bulges or bone spurs:
X-Rays
- Good for viewing bone abnormalities but not soft tissues.
MRI
- Provides clear pictures of vertebrae, discs, nerves, and ligaments.
CT Scan
- Useful for more detailed vertebral bone imaging.
Specialized Tests
Electrical tests examine nerve function:
Electromyography
- Checks electrical activity in muscles to evaluate nerve damage.
Nerve Conduction Studies
- Measures response speed after electrical stimulation, locating conduction blocks.
Treatment Options
Various conservative treatment approaches may provide relief:
Medications
Drugs help ease inflammatory pain and discomfort:
Oral Pain Relievers
- Over-the-counter non-steroidal anti-inflammatories (NSAIDs) like ibuprofen or naproxen reduce swelling. Stronger narcotic pain pills may be prescribed for severe symptoms.
Muscle Relaxants
- Medications like cyclobenzaprine or tizanidine calm muscle spasms.
Steroid Injections
- Corticosteroids administered into the epidural space around affected nerves help alleviate inflammation.
Physical Therapy
Specific exercises strengthen supportive muscles, improve flexibility, and teach proper movements to prevent further injury. Massage and heat/cold therapies also help.
Spinal Injections
Besides steroid shots, hyaluronic acid injections may replenish cushioning between vertebrae, while nerve block numbing agents reduce localized discomfort.
Surgical Interventions
If conservative measures fail and leg weakness progresses, surgery may be warranted:
Decompression Surgery
A laminectomy or foraminotomy opens areas of impingement around nerves.
Discectomy
- Removing part of a ruptured disc eases pressure on nerve roots.
Spinal Fusion
- Fusing problematic vertebrae together increases stability and reduces nerve irritation.
Alternative Approaches
Some patients find relief from alternative treatments like:
Acupuncture
- Thin needles placed in specific body points may interrupt pain signals.
Yoga/Tai Chi
- Gentle stretching coupled with focused breathing and meditation aids relaxation.
Massage
- Hands-on manipulation eases tense muscles putting pressure on nerves.
Are there Ways to Prevent Spinal Related Leg Pain?
While not all nerve-related leg discomfort can be avoided, certain healthy lifestyle measures minimize risk:
Core Muscle Strengthening
Exercises targeting back extensors, glutes, pelvic muscles, and abdominals stabilize the spine and support proper movement patterns.
Maintaining Good Posture
Poor sitting or standing postures increase strain. Adjust workstations for proper ergonomics, take frequent breaks, and use good form during all activities.
Reaching/Maintaining a Healthy Body Weight
Added weight from obesity stresses the spine. Losing excess pounds prevents wear-and-tear.
Conclusion
In summary, spinal related leg pain describes radiating lumbar nerve symptoms caused by compression, inflammation, structural damage, or injuries irritating nerve roots. Getting an accurate diagnosis through imaging tests, nerve studies, etc. enables targeted treatments to relieve discomfort. While not always preventable, lifestyle measures like core strengthening, weight control, and avoiding spinal strain are key.
Written by Dr. Tony Mork
Orthopedic Spine Surgeon
I’m Dr. Tony Mork, MD, a Minimally Invasive Orthopedic Spine Surgery Specialist in Newport Beach, California. With over 40 years of experience, I’m dedicated to providing information for all topics that involve neck and back pain.
January 26, 2024
Contact a Spine Specialist Near You!
Related Articles
Lower Back Pain | An Overview
Lower back pain is an exceedingly common affliction that affects up to 80% of adults at some point in their lives. Understanding the underlying causes of lower back pain is key to finding the appropriate treatment and relief. Anatomy of the Lower Back The lower back,...
Degenerative Disc Disease | Causes and Risk Factors
Degenerative disc disease describes age-related wear and tear to the rubbery spinal discs cushioning the vertebrae that can lead to chronic back or neck pain. While partly genetic, there are also lifestyle factors and injuries that accelerate disc degeneration over...
Upper (Thoracic) Back Pain | What is Causing My Pain?
Upper back pain is a surprisingly common affliction, affecting up to one-quarter of the adult population at some point. While not as prevalent as lower back pain, discomfort in the thoracic region still accounts for a substantial slice of musculoskeletal complaints...



