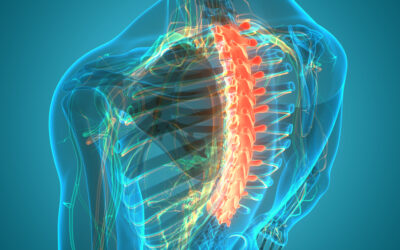
Degenerative disc disease describes age-related wear and tear to the rubbery spinal discs cushioning the vertebrae that can lead to chronic back or neck pain. While partly genetic, there are also lifestyle factors and injuries that accelerate disc degeneration over decades.
As discs progressively dry out, weaken, and develop tears, they lose shock absorbing capacity. This causes nerve inflammation, tiny movements leading to instability, and possible herniation along the spine. Not everyone with disc degeneration feels significant pain or disability. Symptoms arise when cumulative damage finally outpaces the spine’s ability to compensate.
Spinal Anatomy and the Aging Process
Our spine is comprised of 33 vertebrae separated by gel-filled discs that act as shock absorbers while permitting flexibility. Discs contain an inner gel-like core called the nucleus pulposus surrounded by a tough fibrous wall, the annulus fibrosus.
Over a lifetime, discs progressively:
- Lose hydration and internal pressure
- Weaken as tiny cracks and tears develop in the outer wall
- Collapse, flatten or bulge into the spinal canal
This gradual water loss and drying out is part of the natural aging process as nearby blood vessels supplying nutrition to discs deteriorate.
By age 60, over 85% of adults show imaging evidence of disc degeneration, even if asymptomatic. While pain prevalence increases with age, severe disability is more common between ages 30-50 years when more routine activity stresses increasingly damaged discs.
Genetics dictate cellular changes that accelerate disc degradation for some individuals. Environmental factors that overload the spine then incite symptomatic issues in middle age before the spine re-stabilizes.
Genetic Predisposition – Disc Disease Can Run in Families
Twin studies confirm degenerative disc disease has a heritable component, passed from parents to offspring. People with a family history have up to 6 times higher risk of developing disc disease, especially when more closely related.
Molecular studies have uncovered genetic defects involved in disc degeneration including:
- Abnormal collagen formation – Collagen provides structural strength to the outer disc wall that weakens with certain collagen mutations.
- Inflammation regulation – Specific inflammatory genes are overexpressed in people with disc disease.
Such defects don’t guarantee future disc problems, but indicate that some individuals are predisposed to earlier disc issues or more severe pain symptoms when disease develops. Genetics sets susceptibility, while environmental factors then determine progression.
Environmental Stresses: Injury, Strain, Lifestyle
Aging changes spine biomechanics, while genetic weaknesses make discs prone to tear with added stress. Environmental factors provide that final insult tipping genetically vulnerable discs over the edge into symptomatic disease.
Acute Injuries
- Major traumas like fractures, falls, whiplash, and accidents involving blunt force damage to spinal structures.
- Most disc disease instead arises insidiously from periods of overloading the spine in daily life.
Repetitive Strain
- Heavy or repetitive lifting
- Contact sports stressing the neck or back
- Poor posture during laborious jobs or hobbies
- Being overweight – excess body mass strains vertebral joints
- Prolonged sitting stressing spinal discs
Biological Lifestyle Factors
Several health behaviors biologically speed disc breakdown:
- Smoking – Impairs microvascular supply to discs, depriving tissue of oxygen and nutrients needed to maintain structural integrity. Smokers have 300% higher rates of disc degeneration.
- Diabetes – Poor blood sugar control accelerates atherosclerosis. Calcified vessel walls obstruct arterial branches supplying spinal discs.
- Cholesterol – LDL particles damage blood vessels feeding discs through atherosclerotic inflammation and oxidative stress.
Protective Factors
- Exercise – Light resistance and flexibility training strengthens core spinal muscles taking pressure off discs during routine motions. Athletes have lower rates of disc degeneration.
- Healthy Diet – A Mediterranean style diet high in anti-oxidants protects vascular supply to discs and counters systemic inflammation.
In essence, while age-related changes to spinal discs occur inevitably over decades, one’s genetic vulnerabilities and lifestyle largely determine the tipping point into painful dysfunction.
Why Does Disc Degeneration Cause Pain?
Nerves within spinal discs cannot feel pain. So wearing out discs rarely causes hurts. Problems happen when nearby nerves get inflamed due to discs falling apart and spine segments becoming unstable.
Inflammatory Mechanisms
- As the outer wall develops cracks, the inner nucleus can leak inflammatory molecules that directly excite nearby nerve fibers.
- Sensitized nerves then overreact to normal spinal motions, triggering painful spasms.
Structural Instability
- With advanced disc thinning, cushioning capacity decreases during physical activities or postures like sitting.
- Uneven loading and tiny abnormal movements then occur along the spinal segment.
- Localized weakness spurs paraspinal muscles to contract and splint affected areas, often painfully.
Over months-years, a progressively degenerating disc can also:
- Slip out of place (herniate)
- Narrow the spinal canal
- Impinge exiting nerve roots contributing to pain that radiates down the legs or arms.
Symptom Fluctuations Over Time
The clinical picture with spinal disc degeneration varies over decades depending on the balance between accumulating disc damage and the spine’s compensatory responses.
- After an initial precipitating event, pain may linger for weeks to months during local inflammation and segmental instability. Core muscles subsequently strengthen to stabilize vulnerable spinal regions, easing pain.
- Periodic flares then reoccur during activities temporarily overloading the joint’s reduced capacity.
- Over years gradual neural adaptations occur lowering pain intensity. Most older individuals have radiographic spinal disc wear without disabling pain as the spine recalibrates – but smaller insults can still provoke symptoms.
Diagnostic Journey
Imaging modalities like X-rays, CT scans and MRI provide anatomical snapshots clarifying sources of spinal degeneration. However, clinical symptoms do not always neatly correlate with structural deterioration at a given point in time.
When spinal disc disease is suspected, physicians carefully consider:
- Pain characteristics – location, movements aggravating or easing discomfort
- Physical exam findings – nerve dysfunction, muscle spasms
- Family history
- Response to initial conservative treatment
This holistic synthesis of patient factors necessary helps determine whether symptomatic discs or surrounding structures are generating pain.
Preventing Premature Disc Degeneration
Lifestyle measures to avoid injury, foster joint integrity, and hone adaptive capacity powerfully influence the spine’s lifelong functioning. While disc degeneration is inevitable over decades, targeted habits preserve quality years.
Remaining Active
- Low-impact activity strengthens core spinal muscles countering instability from disc thinning. Tai chi, swimming and walking avoid excessive spinal pressures.
- Workplace ergonomics facilitate good posture and regular stretch breaks to decompress the spine.
Muscle Strength
- Building balance, endurance and spinal flexibility via targeted exercise protects vertebral joints from repetitive strain. Just 15-20 minutes daily suffices for benefits.
- Yoga postures improve joint mobility while enhancing muscular support of vulnerable spinal segments prone to instability.
Body Weight
- Losing excess fat reduces spinal disc pressure in the neck and low back. Just 10% weight reduction meaningfully alleviates symptoms of spinal disc degeneration.
Nutrition
- Anti-inflammatory diets high in Omega-3 fatty acids may slow disc dehydration and deterioration by optimizing microvascular circulation supplying spinal tissues.
- Key micronutrients like glucosamine chondroitin, Vitamin D, turmeric and magnesium bisglycinate also preserve age-related cartilage changes and support muscle function surrounding the spine for added stability.
Conclusion
Degenerative disc disease is exceedingly common, yet variably impacts quality of life depending upon genetic, lifestyle and environmental factors interacting over one’s lifespan. Understanding this balance of risks empowers targeting prevention strategies towards maintaining mobility through healthy aging of the spine.
Written by Dr. Tony Mork
Orthopedic Spine Surgeon
I’m Dr. Tony Mork, MD, a Minimally Invasive Orthopedic Spine Surgery Specialist in Newport Beach, California. With over 40 years of experience, I’m dedicated to providing information for all topics that involve neck and back pain.
February 13, 2024
Contact a Spine Specialist Near You!
Related Articles
Lower Back Pain | An Overview
Lower back pain is an exceedingly common affliction that affects up to 80% of adults at some point in their lives. Understanding the underlying causes of lower back pain is key to finding the appropriate treatment and relief. Anatomy of the Lower Back The lower back,...
Upper (Thoracic) Back Pain | What is Causing My Pain?
Upper back pain is a surprisingly common affliction, affecting up to one-quarter of the adult population at some point. While not as prevalent as lower back pain, discomfort in the thoracic region still accounts for a substantial slice of musculoskeletal complaints...
Upper (Thoracic) Back Pain | Understanding Why it Hurts
Upper back pain refers to any type of discomfort or pain in the thoracic spine region. This article will provide an in-depth overview of upper back pain, including its causes, symptoms, diagnosis, and treatment options. We aim to help readers understand the anatomy of...