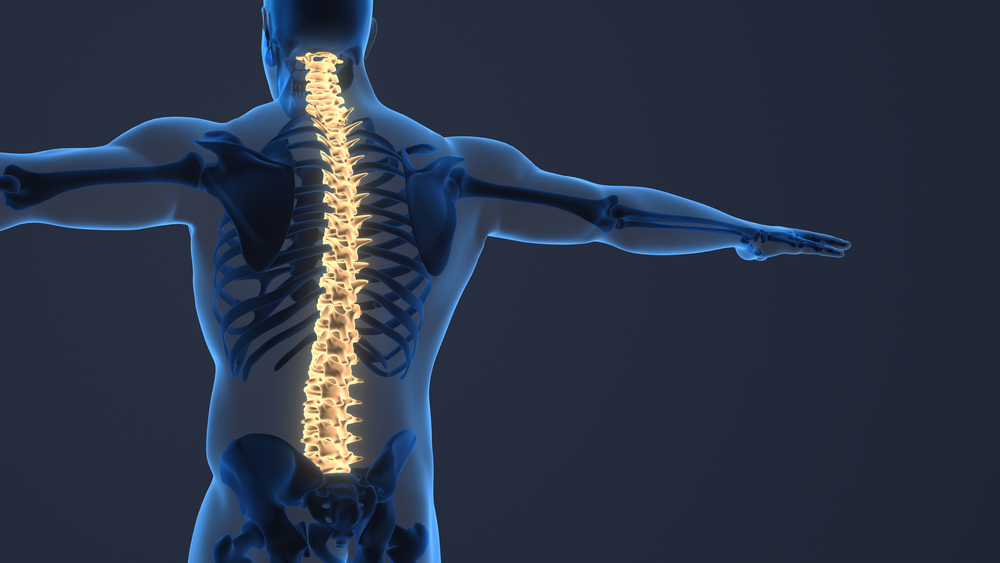
A spinal tumor is an abnormal mass of tissue growth within or surrounding the spinal cord and/or spinal column. These masses can be cancerous (malignant) or noncancerous (benign). Spinal tumors affect individuals of all ages and can cause significant pain and neurological deficits if left untreated. Approximately 30-40% of cancer patients develop spinal metastases during their disease course. Let’s explore these complex growths and current treatment strategies in more detail.
Types of Spinal Tumors
There are two main classifications of spinal tumors – primary tumors that originate in the spine versus secondary metastatic tumors that have spread from cancers elsewhere in the body.
By Spinal Region
The spine consists of cervical (neck), thoracic (mid-back), lumbar (lower back), and sacral regions. Tumors can develop in any of these areas but are most common in the thoracic and lumbar spine.
- Cervical spinal tumors account for 10% of all spinal column tumors. Symptoms may include neck pain, muscle weakness, and loss of bladder control.
- Thoracic spinal tumors represent 45% of all spinal column tumors. Back pain is the most common symptom.
- Lumbar spinal tumors account for 35% of spinal column tumors. Symptoms include lower back pain that radiates down the leg as well as numbness and tingling.
- Sacral spinal tumors such as chordomas are rare but aggressive. They cause localized lower back pain and neurological deficits.
By Location
In addition to spinal region, tumors are characterized based on their location in relation to the spinal cord itself:
- Extradural spinal tumors develop in the vertebrae outside the thin protective spinal cord lining. These account for 55% of spinal tumors.
- Intradural-extramedullary spinal tumors occur inside the spinal cord lining but outside the cord itself, comprising 40% of cases.
- Intramedullary spinal tumors form within the spinal cord, making up 5% of all spinal tumors. These are especially dangerous due to direct damage to spinal cord pathways.
Benign vs Malignant
Benign spinal tumors are noncancerous growths that typically have well-defined borders. Even though they do not metastasize to other sites, benign tumors can still be serious if left untreated.
Malignant spinal tumors are cancerous and carry the ability to spread to other organs and tissues. Some originate in the spine as primary malignancies while the majority represent metastatic deposits from advanced cancers like breast, lung, and prostate carcinomas.
Specific Spinal Tumor Types
There are over 100 types of spinal tumors ranging from common to quite rare. Some of the major categories include:
- Meningiomas: These slow-growing benign tumors arise from the meninges surrounding the spinal cord and nerve roots. They represent 25% of all spinal tumors.
- Schwannomas: These benign nerve sheath tumors can cause neurological deficits as they put pressure on nerve roots.
- Ependymomas: These gliomas come from ependymal glial cells within the central canal of the spinal cord itself. Although usually low grade, they can spread via cerebral spinal fluid.
- Hemangioblastomas: These highly vascular benign tumors arise from blood vessels around the spinal cord and grow via nutrient supply.
- Metastatic cancers: As noted above, metastatic seeding from primary cancers like lung, breast and prostate carcinomas is unfortunately very common, representing 90-95% of malignant spinal disease.
Causes and Risk Factors
The underlying cause behind most primary spinal tumors is unknown. Some may result from genetic conditions or exposure to radiation or carcinogens. Spinal injury and chronic inflammation may also promote tumor growth.
Secondary metastatic spinal lesions originate from a primary cancer elsewhere in the body. Cancer cells break off the original tumor site, enter the bloodstream, and get deposited in the vertebrae or spinal tissues.
Those already diagnosed with cancer or who have first-degree relatives with genetic conditions like neurofibromatosis-2 and Von Hippel Lindau disease are at increased risk for developing spinal tumors.
Symptoms and Diagnosis
The most common initial symptom of both malignant and benign spinal tumors is progressive lower back pain, often severe enough to wake someone from sleep. The pain may radiate to the hips, legs or arms depending on the spinal level affected and location compressing specific nerve roots.
As spinal tumors grow, they can cause escalating neurological problems including weakness, numbness, tingling, loss of bowel/bladder function, and even paralysis in advanced cases compressing the spinal cord itself. Abnormal gait, repeated falls, and new onset scoliosis may also occur with destructive vertebral lesions.
If a spinal tumor is suspected based on concerning symptoms, prompt imaging is key. MRI provides superb definition of soft tissue and areas surrounding the spinal cord while CT better visualizes bone integrity. A CT myelogram injects contrast dye to give additional detail on compression effects. Imaging can detect tumors as small as 3 mm in many cases.
Finally, the only definitive way to classify a spinal tumor is via biopsy and pathological analysis. This identifies markers differentiating low grade tumors, aggressive malignancies, and metastatic disease. Biopsies can be done by needle for smaller lesions or surgical sampling for larger growths.
Treatment Options
The overarching goals guiding spinal tumor treatment are relieving pain, preserving neurological function, and maintaining spine stability. Unfortunately, many malignant spinal tumors cannot be cured. Their therapy instead focuses on improving quality and longevity of life.
Nonsurgical Approaches
- Active surveillance is reasonable for small, asymptomatic spinal tumors likely benign in nature based on imaging characteristics and clinical judgement. Follow-up MRI monitoring ensures growth stalls.
- Chemotherapy aims to destroy cancerous cells with cytotoxic drugs. This can shrink tumors prior to surgical resection and help prevent further metastatic spread.
- Radiation uses targeted beams of high energy X-rays focused on the tumor. This elicits DNA damage and subsequent tumor cell death. Stereotactic radiosurgery allows even more precise conformal doses. 30 Gy over 10 sessions is standard.
- Cement augmentation procedures like vertebroplasty and kyphoplasty involve injection of bone cement to stabilize collapsed vertebrae after tumor destruction. By preventing further compression, they relieve pain and help patients return to daily activities.
- Medications like steroids, anti-inflammatories, and narcotics can help manage spinal tumor symptoms though should not replace definitive treatment.
Surgical Treatment
Surgical removal of spinal tumors has a few general indications including tissue diagnosis in uncertain cases, spinal instability, failure of radiation/chemotherapy, clear neurological deterioration (particularly bowel/bladder involvement), and intractable pain despite conservative measures. Goals of open resection include total en bloc removal wherever safely feasible based on tumor type and location. Any gaps are filled via spinal instrumentation and bone grafting for segmental fusion.
Minimally invasive spine surgery techniques allow access through smaller incisions leading to quicker recovery in appropriate cases when total resection is unlikely. The prognosis following spinal tumor surgery relates to the degree of resection achieved and overall cancer staging. Regular postoperative MRI surveillance monitors for tumor recurrence. Physical therapy helps patients regain mobility.
Special Considerations
There are a few unique concerns regarding spinal tumors in certain populations that alter diagnostic and treatment considerations:
- For pediatric spinal tumors, the emphasis is placed on preservation of vertebral growth centers wherever possible to avoid future deformity. Bracing often supplements surgery. Chemotherapy sensitizes young bodies more so dosage adjustments are needed.
- During pregnancy, the risks posed by adjuvant chemotherapy and radiation generally outweigh benefit except in highly aggressive cases. Some back tumors can safely wait for fetal delivery prior to intervention unless severe neurological decline develops.
- There are great online/in-person support communities for those suffering from spinal cancer to help them share stories and feel connected through an emotionally difficult diagnosis. Seeing successful survivorship cases boosts mental wellbeing.
Living with Spinal Tumors
Even after receiving a spinal tumor diagnosis and completing initial therapy, most patients benefit from coordinated care guiding rehabilitation, monitoring for recurrence, and addressing symptoms/side effects as they arise:
- Follow up MRIs are done at regular 6 month intervals matching surveillance protocols based on the tumor histological grade and propensity for seeding metastases.
- Physical and occupational therapy slowly build back flexibility, core strength, and balance control. This prevents falls/injuries and speeds mobility. Aerobic training fights deconditioning from steroid use. A brace can supplement healing post-operatively.
- Medications effectively manage tumor associated neuropathic pain which may persist. Anti-inflammatories reduce swelling while narcotics provide analgesic relief during severe flares.
- Nutritional guidance ensures adequate caloric intake for wound healing after anti-cancer treatments. Supplements correct common vitamin deficiencies.
- Social workers facilitates home care resources.
The emotional toll of spinal cancer can also run high. Support groups allow patients to process their diagnosis while selective counseling addresses mood disorders, especially depression and anxiety.
Patients living with spinal tumors see multidisciplinary care teams including neurosurgeons, medical/radiation oncologists, radiologists, pain specialists, primary care providers, therapists, nutritionists, and palliative medicine. This level of support provides the best chance for an optimal, empowered quality of life.
Conclusion
Spinal tumors comprise a diverse collection of pathologies with complex symptoms and management considerations:
- They can arise primarily or represent secondary metastases from common systemic cancers like breast, prostate & lung carcinomas.
- MRI and CT imaging followed by tumor biopsy are key for accurate classification and staging which guides treatment.
- Back pain with progressive neurological deficits warrants prompt specialist referral for urgent diagnosis and intervention.
- Goals revolve around alleviating pain, preserving neurological function, maintaining spine stability and improving patient quality/longevity of life.
- Options range from active surveillance to chemotherapy, radiation therapy, cement augmentation, and open surgical resection with reconstruction.
- Even after treatment, coordinated supportive care manages recurrence surveillance, rehabilitation, symptom control, nutrition and emotional support.
Catching tumors early when surgical cure remains viable offers the best outcomes. Patients should have an empowered voice in their care decisions. While at times the road proves difficult, there are always caring professionals ready to walk alongside you.
Written by Dr. Tony Mork
Orthopedic Spine Surgeon
I’m Dr. Tony Mork, MD, a Minimally Invasive Orthopedic Spine Surgery Specialist in Newport Beach, California. With over 40 years of experience, I’m dedicated to providing information for all topics that involve neck and back pain.
February 6, 2024
Contact a Spine Specialist Near You!
Related Articles
Lower Back Pain | An Overview
Lower back pain is an exceedingly common affliction that affects up to 80% of adults at some point in their lives. Understanding the underlying causes of lower back pain is key to finding the appropriate treatment and relief. Anatomy of the Lower Back The lower back,...
Degenerative Disc Disease | Causes and Risk Factors
Degenerative disc disease describes age-related wear and tear to the rubbery spinal discs cushioning the vertebrae that can lead to chronic back or neck pain. While partly genetic, there are also lifestyle factors and injuries that accelerate disc degeneration over...
Upper (Thoracic) Back Pain | What is Causing My Pain?
Upper back pain is a surprisingly common affliction, affecting up to one-quarter of the adult population at some point. While not as prevalent as lower back pain, discomfort in the thoracic region still accounts for a substantial slice of musculoskeletal complaints...



