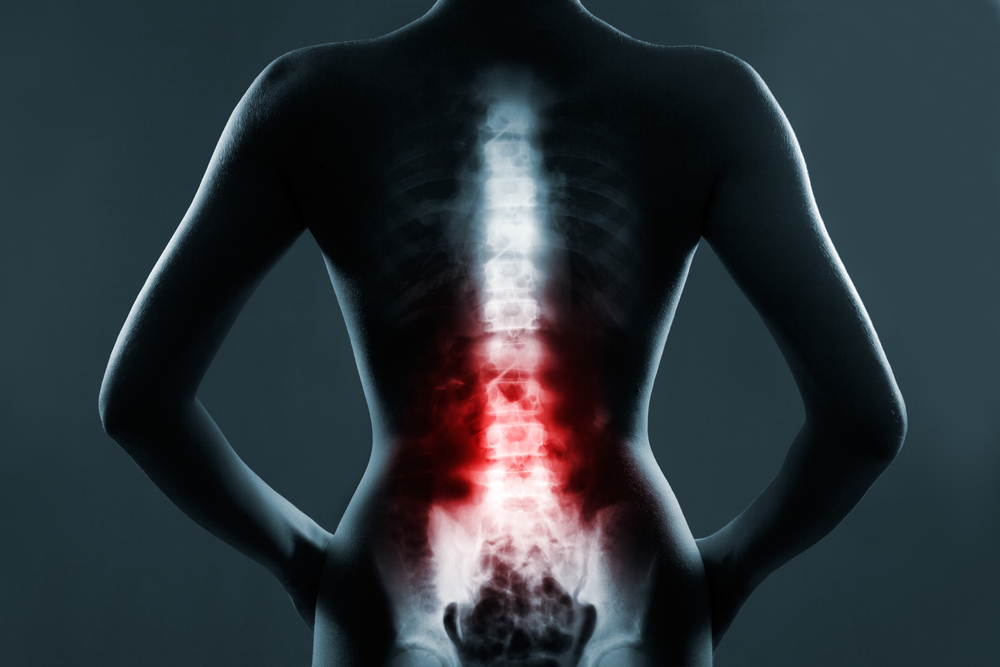
Spinal arthritis is inflammation affecting the facet joints between vertebrae in the spine. It can lead to significant back and neck pain, reduced mobility, and neurological symptoms. With proper diagnosis and treatment, most people with spinal arthritis can manage their symptoms and remain active.
Types of Spinal Arthritis
There are several types of spinal arthritis, with different underlying causes:
Osteoarthritis
Osteoarthritis (OA), sometimes called degenerative disc disease, is the most common type of arthritis overall and in the spine. In OA, the cartilage cushioning the joints slowly wears away over time, leading to inflammation, pain, and stiffness.
Causes: Primary OA has no single identifiable cause, but results from years of everyday wear and tear on the joints. Factors like age, joint injury, obesity, and genetics play a role.
Location: Osteoarthritis most often affects the neck (cervical region) and lower back (lumbar region), as these areas withstand the most movement and stress.
Prevalence: Experts estimate up to 95% of adults over 60 have some degree of spinal osteoarthritis.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an inflammatory autoimmune disease where the body’s immune system mistakenly attacks healthy joint tissues.
Origin: In RA, inflammation is caused by an abnormal immune response rather than mechanical damage.
Cervical involvement: RA frequently affects the cervical spine (neck region).
Gender differences: Rheumatoid arthritis is more common in women than men.
Spondyloarthritis
Spondyloarthritis refers to a family of inflammatory arthritic conditions that cause bone destruction and fusing in the spine and other joints. Examples include:
Ankylosing spondylitis: This progressive form of arthritis causes inflammation in the spine and sacroiliac joints, sometimes resulting in a fused, hunched posture.
Psoriatic arthritis: Occurring in those with the skin condition psoriasis, this can cause arthritis throughout the body, including the spine.
Reactive arthritis: Joint inflammation triggered by an infection elsewhere in the body. Typically arises in the lower spine and improves on its own.
Enteropathic arthritis: Arthritis associated with inflammatory bowel disease, flaring concurrently with IBD symptoms.
Axial vs. peripheral: Spondyloarthritis affecting the spine and sacroiliac joints is considered axial. Involvement of shoulders, hips, hands, and feet is termed peripheral.
Symptoms and Diagnosis
Common spinal arthritis symptoms include:
Symptoms
- Back or neck pain
- Stiffness, reduced flexibility
- Grinding sensation with movement
- Arm/leg pain or numbness
- Headaches
- Fatigue
Diagnosing spinal arthritis involves:
Diagnostic Tests
Imaging: X-rays, MRIs, CTs detect joint damage and rule out other causes.
Physical exam: Range of motion tests, areas of tenderness identified.
Lab tests: Check for markers of inflammation or autoimmunity.
Joint aspiration: Analyzing spine joint fluid for signs of inflammation.
Causes and Risk Factors
Many factors can increase one’s risk of developing spinal arthritis, there are multiple different causes:
Osteoarthritis Causes
Primary osteoarthritis of the spine develops gradually due to:
- Years of normal wear and tear
- Prior joint injuries
- Excess weight placing mechanical strain on joints
- Age-related changes in cartilage
- Possible genetic factors
Inflammatory Arthritis Causes
The immune system plays a central role in inflammatory forms like rheumatoid and psoriatic arthritis. Known triggers include:
- Autoimmune dysfunction
- Bacterial, viral, or fungal infections
- Other inflammatory diseases like IBD
Other Arthritis Risk Factors
Beyond causes, other risks include:
- Age
- Obesity
- Sex assigned at birth
- Family history
- Occupation – physically demanding jobs
Careful control of modifiable risks like diet and exercise habits may reduce likelihood of symptomatic disease.
Treatment and Management
While not curable, various treatments can effectively manage spinal arthritis:
Medications
- NSAIDs to alleviate inflammation and pain
- Corticosteroids – potent anti-inflammatories
- DMARDs (disease-modifying antirheumatic drugs) used for inflammatory arthritis
Alternative Therapies
- Physical therapy – improves strength and mobility
- Chiropractic adjustments
- Lifestyle changes – losing weight, posture correction
Surgery
- Decompression – removing tissue pressing on nerves
- Spinal fusion – permanently joining vertebrae to stabilize
Minimally invasive keyhole procedures reduce injury risk and recovery times. As a last resort when conservative measures fail, surgery can provide lasting pain relief.
Prevention
While spinal arthritis cannot always be prevented, protective lifestyle measures include:
Exercise: Staying active keeps joints flexible and strengthens supportive muscles. Low-impact activities like walking, swimming, and yoga are ideal.
Weight management: Maintaining a healthy body weight minimizes unnecessary strain on the spine.
Posture: Using proper posture reduces mechanical stress during daily activities. Consider occupational therapy guidance.
Avoiding occupational overuse through frequent breaks, spacing heavy lifts, and using correct techniques protects the spine from injury. Assistive equipment like lumbar supports helps prevent extra damage.
Though not always possible to prevent, these strategies promote joint health and functioning.
Complications
Without treatment, spinal arthritis can lead to complications including:
Spinal stenosis – narrowing of the spinal canal presses on nerves
Pinched nerves – impingement of nerves exiting the spine causes pain
Fractures – weak, brittle vertebrae due to osteoporosis increase fracture risk
Deformities – hunched posture or kyphosis over time due to erosion and fusing
Prompt diagnosis and tailored therapy helps prevent permanent spinal damage before these issues progress.
Prognosis and Outlook
The prognosis for spinal arthritis varies significantly based on individual factors. While rarely an imminently life-threatening condition, some general expectations include:
Symptom management – Most people achieve substantial control of arthritis pain and stiffness with conservative treatment, allowing normal activity.
Activity levels – Regular exercise and a healthy lifestyle aid strength and flexibility. Pacing activities prevents overdoing it.
Disease monitoring – Periodic imaging helps assess arthritis progression, which may accelerate with age or non-use.
Follow-up care – Worsening, persistent symptoms warrant medical attention to modify therapies as needed. Spinal changes also increase risks associated with certain pain medications.
So, while spinal arthritis cannot be eliminated, prognosis remains positive in the majority patients able maintain activity through an appropriate treatment plan and self-care.
Final Thoughts
Managing spinal arthritis requires patience and perseverance, but significant relief is often attainable through safe exercise, medication when necessary, and healthy lifelong habits. Working closely with one’s care team brings about the best results – especially if caught early. While some pain or stiffness may persist, appropriate treatment keeps most patients on the move. There is hope!
Written by Dr. Tony Mork
Orthopedic Spine Surgeon
I’m Dr. Tony Mork, MD, a Minimally Invasive Orthopedic Spine Surgery Specialist in Newport Beach, California. With over 40 years of experience, I’m dedicated to providing information for all topics that involve neck and back pain.
January 25, 2024
Contact a Spine Specialist Near You!
Related Articles
Lower Back Pain | An Overview
Lower back pain is an exceedingly common affliction that affects up to 80% of adults at some point in their lives. Understanding the underlying causes of lower back pain is key to finding the appropriate treatment and relief. Anatomy of the Lower Back The lower back,...
Degenerative Disc Disease | Causes and Risk Factors
Degenerative disc disease describes age-related wear and tear to the rubbery spinal discs cushioning the vertebrae that can lead to chronic back or neck pain. While partly genetic, there are also lifestyle factors and injuries that accelerate disc degeneration over...
Upper (Thoracic) Back Pain | What is Causing My Pain?
Upper back pain is a surprisingly common affliction, affecting up to one-quarter of the adult population at some point. While not as prevalent as lower back pain, discomfort in the thoracic region still accounts for a substantial slice of musculoskeletal complaints...



