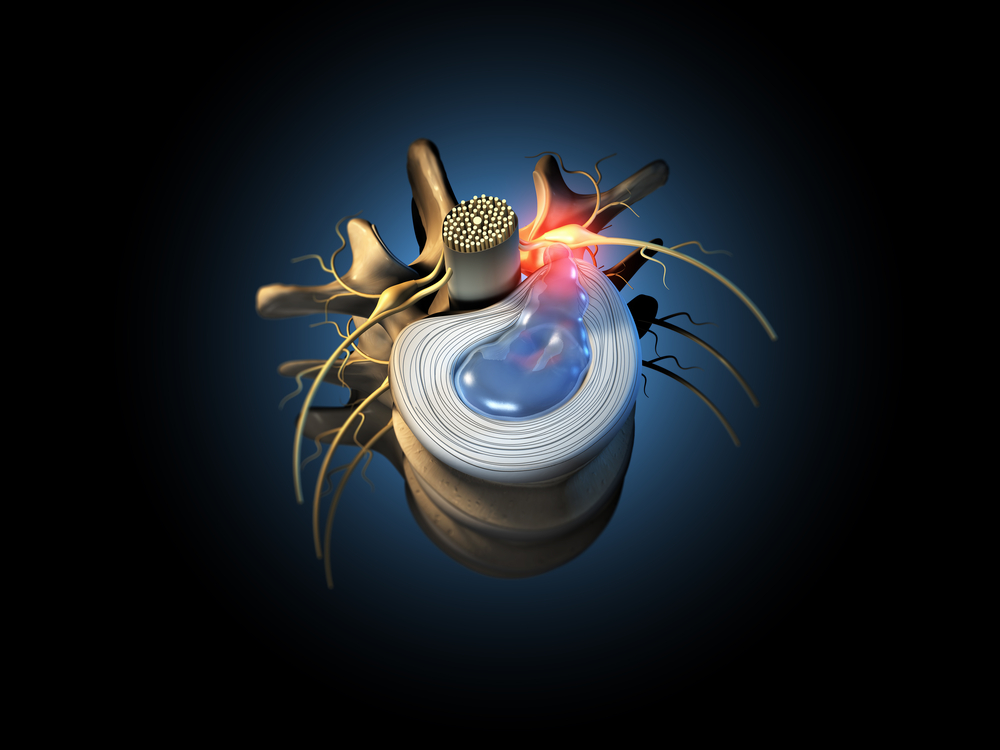
A herniated disc, also referred to as a slipped or ruptured disc, is a painful condition where the jelly-like center of an intervertebral disc pushes out through a weakened area in the outer layer.
Anatomy and Function of Spinal Discs
The spine is composed of 24 interlinking bones called vertebrae, cushioned in between by flexible discs. These intervertebral discs act as shock absorbers and allow the spine to move in different directions.
Each disc has two components – a soft, gelatinous inner portion called the nucleus pulposus, and a tougher exterior ring called the annulus fibrosus. When the tough exterior ring becomes weakened or damaged and the inner nucleus seeps through it, this results in a herniated disc.
Herniated Disc Overview
As you age, the discs in your spine gradually lose water content and flexibility. This natural degenerative process can lead to tears in the outer annulus layer, causing the inner nucleus to push through, herniating the disc. This more commonly occurs in someone over 30 years of age.
Not all herniated discs are the same. There are different degrees of disc herniations based on the severity of the damage and the amount of disc material that leaks through. In a bulging disc, the exterior ring extends outwards but doesn’t rupture completely. A small rupture may result in a protruding disc. The most serious form is an extruded disc when a fragment of nucleus material breaks off entirely into the spinal canal.
As a herniated disc presses on the surrounding nerves, it can trigger pain, numbness, and weakness down the arms or legs depending on the location of the disc. Nonspecific lower back pain without these neurological symptoms could indicate a less severe bulging disc that isn’t touching a nerve.
Causes and Risk Factors
There are various factors that can make someone more susceptible to developing a herniated disc:
Genetics and Family History
Some individuals have genetic mutations and biological factors that contribute to premature disc degeneration. If you have a close family member with degenerative disc disease or herniated discs, you may be at higher risk.
Age and Gender
As we established earlier, disc degeneration increases with age as the discs progressively lose their integrity. Thus, men between the ages of 30 to 50 along with older adults in general are the demographic most vulnerable to herniated discs.
Lifestyle Factors
Certain lifestyle factors substantially contribute to one’s risk of herniation, specifically:
Improper Lifting and Twisting
Forceful lifting with the back and spinal twisting motions are major causes of disc herniations. Such movements overstrain the spine, leading to small tears in the annulus that allow the disc to herniate. Using proper lifting techniques that rely on the legs instead of the back can massively decrease the chances of disc injury.
Weight and Obesity
Excess weight places extra compressive loads on the spine and increases intradiscal pressure, accelerating degenerative changes and annular tears. For this reason, an individual who is obese or overweight is at much higher risk of developing damaged and herniated discs. Losing weight relieves mechanical stress on the discs.
Smoking
Smoking limits blood flow to spinal discs, reducing oxygen and nutrient supply. Over time, this causes accelerated disc degeneration and higher disposition for herniated disc injuries. Quitting smoking can slow this degenerative process.
Sedentary Lifestyle
Lack of core muscle conditioning makes the spine more vulnerable to strains and injuries. Having strong core and back muscles provides crucial support and stabilization to the vertebral column and protects the discs.
Physically Demanding Jobs
Jobs involving repetitive heavy lifting, pushing/pulling, bending, and driving boost one’s odds of disc herniation due to cumulative spinal microtraumas. Cushion-driver interface within truckers and prolonged sitting during work commutes can also degrade spinal discs over months to years.
Degenerative Disc Disease
While expected low-grade age-related disc degeneration isn’t too problematic, some individuals develop severe degenerative disc disease in their 30’s or 40’s from various combinations of genetic and lifestyle factors. Multiple herniated discs are often accompanied by other spinal issues in such cases. Managing controllable risk factors to prevent rapid disc degeneration is key.
Injuries and Trauma
Sudden back injuries from events like falls, accidents, or sports can cause tears in even healthy discs leading to acute high-grade herniations. Though not as common as wear-and-tear or degenerative herniations, traumatic herniations warrant prompt diagnosis and management.
Diagnosis and Testing
An accurate diagnosis begins with a medical history accounting for risk factors and thorough physical examination to characterize the symptoms. Imaging studies are often required to assess spinal structure and confirm disc pathology.
Physical Exam and Medical History
The physician will inquire about any family history and lifestyle habits that could be accelerating disc degeneration. Then they will attempt to reproduce the patient’s arm/leg symptoms through range of motion testing and evaluate any neurological deficits indicating nerve compression. This data steers diagnosis and rules out alternative conditions.
Imaging Tests
Since multiple spinal problems generate similar symptoms, radiographic examination is imperative to directly visualize the discs and pinpoint the anatomical problem.
Common imaging modalities include:
X-ray
Only useful to rule out spinal fractures and alignment abnormalities. Limited utility in diagnosing soft tissue spinal pathology like disc herniations.
MRI Scan
The gold standard imaging modality due to its unparalleled resolution of spinal muscular, disc, ligamentous, and neural structures without radiation exposure.
CT Scan
Best for assessing bony anatomy. May be favored if MRI contraindicated or for preoperative planning before complex spinal reconstruction procedures.
Myelogram
Involves intrathecal contrast injection to outline the spinal canal and discs on X-rays or CT scans. Reserved for inconclusive MRI cases due to its invasiveness.
Other more specialized tests like discography (disc injection) or electromyography may provide supplementary diagnostic information if the main imaging workup fails to establish a clear basis for the symptoms.
Treatment Options
While herniated discs sometimes heal and shrink on their own over time, treatment is often necessary to manage pain and prevent any progressive neurological deficits in the interim. The approach depends on symptom severity and duration but aims to alleviate inflammation and mechanical compression afflicting the neural structures.
Conservative Measures
For acute cases without major neurological deficits, a 4-6 week trial of nonsurgical management improves symptoms in over 90% patients. Components of conservative treatment include:
Medications
Oral NSAIDs, muscle relaxants, neuropathic agents, and narcotics for short-term pain relief. Localized epidural steroid injections can also temporarily reduce discogenic and nerve root inflammation.
Physical Therapy
PT strengthening regimens alleviate symptoms long-term by improving lumbar-core stability to take pressure off damaged discs.
Alternative Therapies
Chiropractic, massage, acupuncture, and Yoga may benefit certain patients if overseen by licensed specialists.
If intolerable pain or neurological compromise on exam persists beyond 6 weeks despite nonsurgical care, surgical intervention may be warranted.
Surgical Options
Main surgical options include:
Discectomy
Removes the protruding disc fragment compressing the nerve to decompress the neural elements and alleviate corresponding leg pain. Preferred 1st option due to least invasiveness and high efficacy.
Laminectomy
Involves additional removal of the vertebral lamina causing stenosis to increase available space if there is concurrent central canal narrowing compromising the nerves or spinal cord.
Spinal Fusion
Joins affected intervertebral segment with metal hardware and bone graft. Improves stability but sacrifices flexibility at fused levels.
Disc Replacement
Total disc prosthesis preserves motion unlike fusion while replacing damaged discs. Comparable outcomes to fusion and may yield better long-term function.
The risks and projected benefits of each modality are weighed appropriately on a case-by-case basis to select ideal surgical candidates and optimal intervention type.
Preventing Herniated Discs
Strategies to deter the development of symptomatic herniated discs center on shielding the spine from excessive strain by building muscular support, maintaining healthy weight, avoiding occupational overuse, and reducing contributory vices like smoking.
Core Strengthening and Safe Lifting
Isometric core exercises improve lumbar stability and prevent excessive loading on discs during routine activities. Squat lifting with straight back also safeguards discs better than bent-over lifting.
Weight Loss
Reduces vertical compressive forces on the lumbar discs, alleviating risk of herniation especially for overweight individuals. Even a 10-15 lb weight reduction can substantially ease mechanical burden on the lower back.
Smoking Cessation
Critical to impede accelerated disc degeneration since smoking hinders vascular supply to the metabolically active discs. Kicking the habit preserves disc integrity.
Job Modification
Altering occupational routines to incorporate more motion variation, frequent breaks, and ergonomic equipment can protect workers prone to overuse spinal injuries.
Those with suspected herniated discs should promptly consult a spine specialist to accurately determine required treatments to alleviate painful symptoms and improve quality of life while working to shield the spinal discs from further harm.
Conclusion
Herniated discs can arise from an array of causes – while aging and genetics play a role, much of one’s risk derives from lifestyle factors like improper lifting, obesity, smoking, and overall spinal overuse. Understanding the various contributors to disc damage allows individuals to make sensible lifestyle adjustments to preserve back health by building core muscle strength, maintaining healthy body weight, utilizing proper lifting mechanics, quitting smoking, and avoiding occupational overexertion of the spine. When herniated discs do occur, being aware of the typical symptoms can clue patients into promptly seeking assessment to access appropriate conservative treatments or surgical solutions and prevent any long-term neuropathy. With mindful lifestyle choices and timely care for any disc disease, one can aim to reduce pain and dysfunction from these common spinal ailments.
Written by Dr. Tony Mork
Orthopedic Spine Surgeon
I’m Dr. Tony Mork, MD, a Minimally Invasive Orthopedic Spine Surgery Specialist in Newport Beach, California. With over 40 years of experience, I’m dedicated to providing information for all topics that involve neck and back pain.
January 25, 2024
Contact a Spine Specialist Near You!
Related Articles
Lower Back Pain | An Overview
Lower back pain is an exceedingly common affliction that affects up to 80% of adults at some point in their lives. Understanding the underlying causes of lower back pain is key to finding the appropriate treatment and relief. Anatomy of the Lower Back The lower back,...
Degenerative Disc Disease | Causes and Risk Factors
Degenerative disc disease describes age-related wear and tear to the rubbery spinal discs cushioning the vertebrae that can lead to chronic back or neck pain. While partly genetic, there are also lifestyle factors and injuries that accelerate disc degeneration over...
Upper (Thoracic) Back Pain | What is Causing My Pain?
Upper back pain is a surprisingly common affliction, affecting up to one-quarter of the adult population at some point. While not as prevalent as lower back pain, discomfort in the thoracic region still accounts for a substantial slice of musculoskeletal complaints...



