A herniated disc occurs when there are tears in the outer annulus fibrosus, allowing the soft inner nucleus pulposus to leak out. This material can press on nerve roots, like jelly squeezing out of a doughnut. Compression and inflammation of the nerves leads to symptoms like pain, numbness and tingling. This painful condition often arises from age-related disc degeneration.
Herniations develop more often in lower spine discs bearing lots of weight. While caused occasionally by injuries, such as falls, most arise simply through age degenerating connective tissues in discs.
Understanding spine anatomy and what contributes to disc injuries allows prevention and informed treatment options.
Spine Anatomy
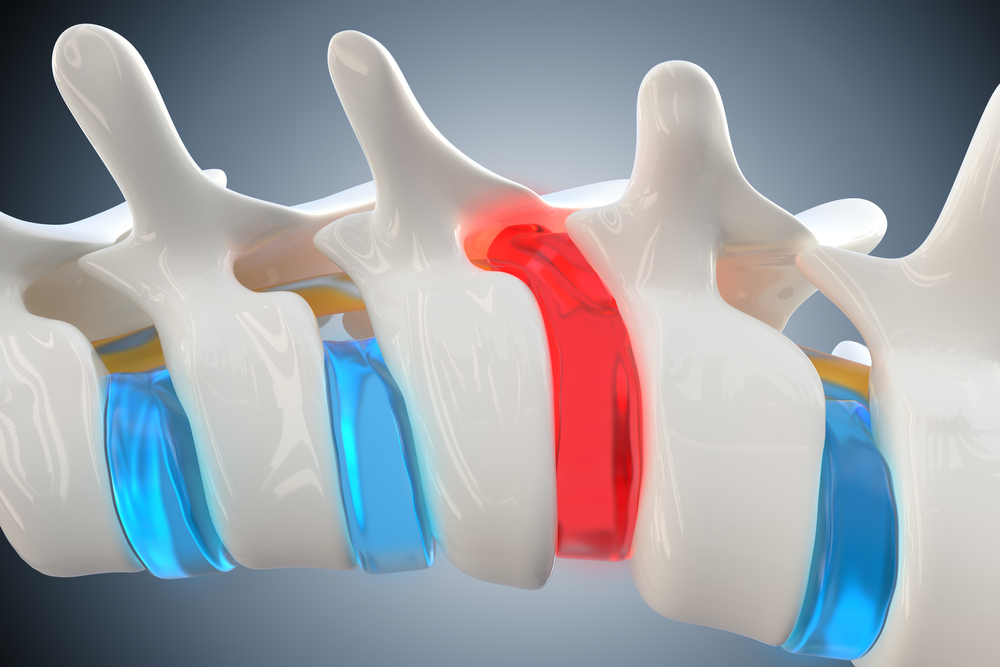
The spine is made of 24 small bones called vertebrae stacked in a column from skull to pelvis, housing and protecting the spinal cord. Between vertebrae are thick, rubbery discs that cushion impact.
Vertebrae
Vertebrae interlock using Facet joints and processes resembling little wings. Together they form a canal to enclose the spinal cord and openings letting spinal nerves exit to the body.
The lower lumber vertebrae bear the most weight. Their size and strength support our upright posture. Damage here has big impact.
Intervertebral Discs
Sandwiched snugly between vertebrae, intervertebral discs act like shocks absorbing pressure. They’re a half inch thick, with tough outer rings called Annulus Fibrosus sealing soft Nucleus Pulposus gel inside.
The nucleus pulposus has a fluid, gelatinous texture that cushions the vertebrae and facilitates smooth movement between them. Over time, degenerative changes can cause tears in the annulus fibrosus, allowing the nucleus material to leak out. When the disc contents press on nerves, it produces symptoms of a disc herniation..
Disc Anatomy – Nucleus and Annulus
Intervertebral discs contain two key parts that enable both cushioning impact and injury when one component weakens. Let’s break it down.
Nucleus Pulposus
This clear, gelatinous proteoglycan center of discs consisting largely of water acts like a fluid ball bearing, distributing between vertebrae for smooth compression and rebound during movement.
Annulus Fibrosus
Made of tough, collagen fibers arranged in rings, this strong flexible barrier wraps securely around gel Nucleus, sealing it in place between vertebrae through connective tissue scar called Sharpey’s fibers.
As part of the natural aging process, the collagen fibers that make up the annulus fibrosus slowly fray and weaken over time. This leads to small tears developing in the outer barrier of the disc. Through these tears, the soft inner nucleus pulposus can leak out when the disc is injured or strained. This event is termed a disc herniation. When disc material presses on adjacent nerve roots, it causes inflammation and irritation, leading to characteristic symptoms.
Herniation Causes and Contributors
There are a few key factors making herniations more likely over time. Understanding these allows strategic prevention so we remain active long term.
Age-Related Disc Degeneration
Like tread wearing thin, ongoing compression forces and injury from daily wear and tear causes tiny fissures in Annulus Fibrosus. Over decades, discs flatten and crack more easily. Genetics plays a part in rate of degeneration.
Improper Lifting and Bending
Twisting and turning while lifting heavy weights or loads puts extra strain on the annulus fibrosus. Over time, repetitive motions like this can cause microscopic tears and wear down discs, causing them to thin and weaken.
Excess Weight
Carrying excess body weight, especially around the abdomen, increases the repetitive loading and compression forces on the spine with daily activities. This greatly accelerates disc degeneration over time, particularly in the lumbar region which bears the brunt of weight bearing stress.
Nutrition and Lifestyle
Just as muscles and ligaments need nutrition, discs rely on hydration, nutrients and oxygen conveyed through blood vessels in vertebrae sandwiching them. Smoking impairs circulation, hastening disc degeneration.
Signs and Symptoms
Symptoms arise from inflammation and compression when disc material leaks out, pressing nerves. This depends on location along the spine column.
Lower Back Herniations
Majority occur in lumber discs bearing most weight. Local pain swells first, then shoots down legs as sciatic nerves get pinched exiting spine canal. Numbness and tingling follows.
Herniations Higher Up
Neck and upper back herniations compress nerve roots leaving spinal cord up top. Pain radiates to shoulders and arms. Headaches and dizziness occurs if cranial nerves are pinched.
If the herniated disc severely compresses the nerves that regulate bowel, bladder, or movement, urgent surgery may be necessary to decompress those nerves and prevent irreversible loss of functionality from prolonged pinch.
Diagnosis and Treatment
To correctly diagnose, physicians conduct a physical analysis of pain and sensation changes, combined with CT scans or MRIs pinpointing disc injuries visually.
Most mild ruptures heal through rest and conservative treatment like anti-inflammatory medication, physiotherapy, chiropractic adjustments or spinal injections. More severe herniations sometimes warrant surgery to remove material pressing nerves. Outcomes are generally positive. Most patients see great improvement in 6-12 months. Understanding prevention is key.
Conclusion
Herniated discs arise commonly through age-related disc degeneration and cumulative impact from daily loading. Learning proper spine mechanics allows strengthening support structures. Losing excess weight minimizes compression forces. Though some herniations occur despite best efforts, prevention and non surgical treatment lessen risk for lasting disability.
Written by Dr. Tony Mork
Orthopedic Spine Surgeon
I’m Dr. Tony Mork, MD, a Minimally Invasive Orthopedic Spine Surgery Specialist in Newport Beach, California. With over 40 years of experience, I’m dedicated to providing information for all topics that involve neck and back pain.
January 25, 2024
Contact a Spine Specialist Near You!
Related Articles
Lower Back Pain | An Overview
Lower back pain is an exceedingly common affliction that affects up to 80% of adults at some point in their lives. Understanding the underlying causes of lower back pain is key to finding the appropriate treatment and relief. Anatomy of the Lower Back The lower back,...
Degenerative Disc Disease | Causes and Risk Factors
Degenerative disc disease describes age-related wear and tear to the rubbery spinal discs cushioning the vertebrae that can lead to chronic back or neck pain. While partly genetic, there are also lifestyle factors and injuries that accelerate disc degeneration over...
Upper (Thoracic) Back Pain | What is Causing My Pain?
Upper back pain is a surprisingly common affliction, affecting up to one-quarter of the adult population at some point. While not as prevalent as lower back pain, discomfort in the thoracic region still accounts for a substantial slice of musculoskeletal complaints...



